Devices for Epilepsy
Approximately 30% of patients with epilepsy continue to have seizures despite trying several antiepileptic drugs (AEDs). This 30% of patients is considered to have intractable epilepsy. Some of these patients can have surgery for their seizures- this is where a surgeon removes a piece of brain tissue to remove the seizure focus. This type of surgery can be very helpful—in some cases, > 70% of patients would be expected to be seizure free.
So, what about the patients who do not respond to seizure medications and also are not resective surgery candidates? What do they do? Such patients may be considered for a device to treat their seizures. A device for epilepsy is something that is placed into a patient by a surgeon. The device is programmed to perform a function that stops seizures.
So, what about the patients who do not respond to seizure medications and also are not resective surgery candidates? What do they do? Such patients may be considered for a device to treat their seizures. A device for epilepsy is something that is placed into a patient by a surgeon. The device is programmed to perform a function that stops seizures.
Currently, there are three devices for epilepsy that are commonly discussed. Only one is FDA approved—this is the Vagus Nerve Stimulator. The other two (Deep Brain Stimulator and Neuropace) are not fully FDA approved. At this time, the Vagus Nerve Stimulator can be ordered by your clinicians. Deep Brain Stimulator and Neuropace are not fully FDA approved and are thus not available to the general public.
A brief description of each of these three devices may be of interest:
Vagus Nerve Stimulator (VNS)
How it works: A battery is placed under the skin on the left side of the chest. A wire goes from this battery to the vagus nerve—this is a large nerve in the neck. Thus, the patient has two areas of surgery- 1) the skin on the left side of the chest and 2) the left side of the neck to attach wires to the vagus nerve. No brain surgery is done. The vagus nerve has connections to the brain—in a widespread manner. The battery produces electrical charge that is transmitted to the vagus nerve. This electrical stimulation is then transmitted to the brain. The device is often programmed to stimulate for 30 seconds and then be off for 5 minutes. This stimulation goes on like clockwork: 30 seconds on/5 minutes off. By stimulating the vagus nerve, which then stimulates the brain, the seizure potential is changed for the better- seizure control can be improved!
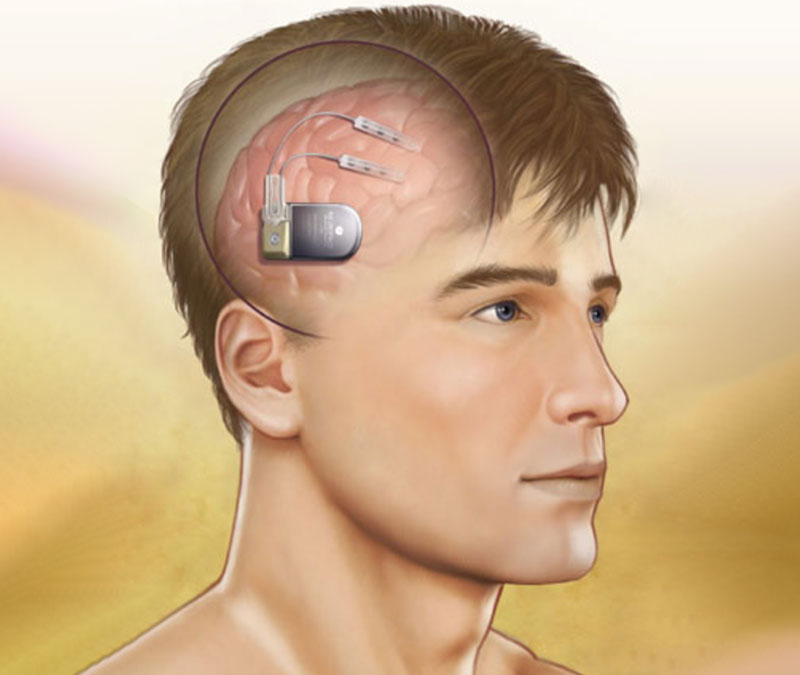
Deep Brain Stimulator
How it works: Small probes are placed deep in the brain. This requires surgery that involves going through the skull and brain tissue. The probes are programmed to delivery electricity to areas deep in the brain. By stimulating this area, the brain activity changes in a good way- seizure activity can be reduced. Like the Vagus Nerve Stimulator, the Deep Brain Stimulator is programmed to stimulate at a pre-programmed set time. For those who love neuroanatomy, the deep brain area is called the anterior nucleus of the thalamus.
Neuropace
How it works: Electrodes are placed on the surface of the brain. This involves brain surgery-a piece of skull is opened to place these electrodes. The electrodes are very sophisticated- they are attached to a computer system that allows the detection of seizure activity. Imagine this- the electrodes are placed directly over the part of the brain where seizures are coming from. When a patient has a seizure, the electrodes can detect this activity. The electrodes are then programmed to delivery electricity to the brain. The electricity from the electrodes zaps the brain—and the seizure activity is stopped!
The three devices described in this article can reduce the frequency and intensity of seizure activity, but they are not expected to stop seizures completely. Obviously, this is important for patients to know. For example, the devices are not expected to stop seizures to the point where patients can drive. Placing one of the above devices may help patients reduce seizure medications. This may help with side effects. The devices would not be expected to produce the well known seizure medication side effects, such as feeling sleepy, dizzy, poor coordination (you know—feeling like you are drugged!).
Each device has its own side effects. When a patient has surgery, infection and stroke are always discussed. Fortunately, the procedures do have a very good safety records.
I will plan on going into more detail about these devices in a future article. I will review the risks and benefits in more detail.
Please comment, ask questions.
For more information:

James White, MD
Dr. White has been practicing as a full-time epileptologist since 1999. His practice focuses on optimizing the diagnosis and treatment of patients with seizure disorders. Dr. White’s special interests include patient education, improving the side-effect profile of seizure medications, and epilepsy surgery.
7 Responses to “Devices for Epilepsy”
B June 21, 2012 at 2:47 pm
Interesting article, thank you for writing. I am wondering about intractable epilepsy in children, specifically young children. What if seizures are of unknown origin as well as “global”, with medication not stopping the seizure activity. How is it determined who a candidate would be, if not VNS then since the others are not FDA approved how or where are they performed if at all? Are these procedures that could help young children two or younger perhaps or more for older children/adults? thank you.

James White, MD June 26, 2012 at 7:37 am
Thank you for your comments. Sorry for my delay–I have been out of the office. Each age group presents its own special challenges: In children less than two years, expertise is needed to clarify the diagnosis. Treatment options–including surgery, is done even in very young children. VNS is FDA approved for those > 12 years of age. There are published articles in the literature describing VNS outcomes in very young children. Outcomes appear to be good. Thank you! James R. White, MD

Greg October 10, 2012 at 11:01 am
Hey doctor – I am 33 and have been having seizures since I was 21. I have been on various medications over the years (current mix is Carbatrol and Lamictal) and two years ago had resective surgery on my right temporal lobe. MSTs were also performed during the surgery.
I was seizure free following surgery for almost six months, but eventually, the seizures broke through again. I still experience 2-3 seizures per month and have not driven in 3 1/2 years.
I’ve sort of been hoping that Neuropace is my magic bullet, so to speak. You mention in your post that none of the three procedures would make a patient seizure free, but what about a person in my case, whose epilepsy is under decent control?
I no longer generalize, which is a good thing. My seizures are all partial complex, but over the past two years have been getting longer and more severe. I recently burned my hand on a hot stove for example, so loss of awareness and loss of motor control definitely present with these partials.
I would love your input. Could Neuropace make me seizure free, assuming I stay on at least one AED? Is it any closer to FDA approval? Incidentally, my neurologist is going to be switching me from Lamictal to Onfi soon. Any thoughts on that? Thanks,
Greg

Alissa Minion January 17, 2013 at 3:43 pm
Any updates as to fda approval on the deep brain stimulator or the neurospace?

Dr. Donald Perman Jr. DMD July 17, 2013 at 11:14 am
I am a dentist who suffered seizures who was on Tegretol and Depicote for 20 years along with Left Temperal Lobe surgery when I was 31. I had one grand mal 18 months later on the floor of the dental clinic of the OHSU dental school.
Two year later removed myself from all medication for over 20 years. Now at age 53 out of the blue with no injury I recently had another grand mal seizure. Any thoughts, I have under normal stress of life and no unusual issues.
Could there be any correlation to the level of mercury intake as I removed a lot of silver fillings last week and had a lot of mercury vapor intake. My only thought, thanks, Don

Marlena King August 8, 2014 at 12:25 am
Dr.Whit My Name is Marlena I have a 5 year old daughter that was diagnosed with Epilepsy when she was 2. She has bin on several different Medications and has bin hospitalize several times. My daughter has seen several Neurologists and has also bin to a level 4 Epilepsy center she is currently on Omfi, Felbamate , Vimpat, Oxcarbenzapine she is very dizzy all the time she use to be a normal size child and very loving now she is almost 100 lbs and is very violent she also hoards food they had focused the VNS as something to try I am really learning as I go but I want to know if this will work better than all these meds I would like any input that you have.

Ida March 18, 2019 at 10:32 am
Dear Dr. White. Thank you for your information It is the best and most up-to-date material I have read. I have a 50-year old family member who is in dire need of help and refuses follow-up and medication. In the wake of a car injury there was brain surgery and several days in a coma 41 years ago. Luckily, the recovery allowed a physically healthy lifestyle but ADHD affected learning and reasoning. Then about 10 years ago there were grand mal seizures at night, usually EMS was called and the hospital went through various diagnostic processes and sent the patient home with prescription and request to follow up. The seizures still happen but are milder and often can be stopped by a gentle touch or stroke of the left arm or the forehead and there is less of the salivation/exudation. My observation is also that the seizures are tied to mental stress and nutrition.

